Please note – the NIHCA is not responsible for the content of any news from outside the NIHCA posted here, the content of any external training provided nor the content of any external links.
Dr Naughton: Clinical pastoral education
is challenging but transformative
Source: https://catholicnews.ie/dr-naughton-clinical-pastoral-education-is-challenging-but-transformative/
“There may be no Sam Maguire in Kerry this summer but this did not stop the celebrations in the kingdom! On 23 July, seven graduates of the Clinical Pastoral Education Programme at University Hospital Kerry completed an intensive twelve-week unit. Clinical Pastoral Education, or CPE as it is more commonly known, has historically been a preparatory programme for hospital chaplaincy. In more recent years its remit has expanded somewhat to include people in preparation for ministry in many other pastoral contexts and situations.
CPE has a focus on the ‘self’ and on the ‘professional’ – supporting participants to grow and develop personally, pastorally and professionally as well as on the multiplicity of skills that are now needed to minister in healthcare facilities (and other pastoral contexts) within an ever-shifting cultural dynamic.
CPE has a trinitarian approach – it consists of education, supervision and clinical placement. Participants are taught many of the skills of listening, how to be present to another person as well as harnessing the gifts of compassion and empathy that are already within the pastoral practitioner. They are also exposed to didactics and workshops on loss, grief, pastoral theology, theology of suffering, hope and many others – helping them to develop skills in reflective practice and theological reflection – core elements of the CPE modality as well as pastoral ministry itself. Students also have weekly individual supervision (as well as group supervision) – a safe space to reflect on their personal, pastoral and professional issues as they emerge during the CPE formation. This is where the CPE methodology of action-reflection-action comes into its own – taking the learnings and insights and bringing them back out into the field so that they can be put into practice. And finally, there is the clinical component of the CPE programme where students encounter ‘living human documents’ – the people who can and do become our best teachers when we learn from the experience of human vulnerability (ours and theirs). Student chaplains are presented with the reality of life and death and in confronting such issues they learn how to be accompany another person in their moments of woundedness and vulnerability.
CPE is a challenging but transformative process. It changes the participants in different ways usually for the better. CPE helps us to learn in real time that sometimes there are no answers, no solutions, nothing that can or will make a difference in the face of real human suffering except our compassion, vulnerability and willingness to show up for another person without judgment, without agenda, without hope of reward.
Dr Margaret Naughton is a Clinical Pastoral Educational Supervisor and Healthcare Chaplain at University Hospital Kerry.
CatholicNews.ie would like to thank Dr Margaret Naughton for submitting this article for publication.”
AGM – Tuesday 28th May
Our 63rd Annual General Meeting takes place on Tuesday 28th May. Registration with tea/coffee and scones opens at 9am with business to begin at 9.30am.
Our AGM is being held in The House of Vic Ryn – T3 Conference Centre, Moira Road, Lisburn. Copies of the Annual Report for 2023-204 will be available on the day.
Please let our training director know by Monday 20th May if you are able to attend and intend to stay for lunch, highlighting any dietary requirements – his email is trainingdirector@nihca.co.uk
Any matter to be raised at the AGM under AOB must be with the Training Director in writing by Tuesday 21st May 2024.
We encourage our members to invite their line managers although appreciate that this may be late notice
Membership Fees for 2024/2025
Membership for 2024/2025 is due. This can be paid in cash before the AGM or on the day. Please note, after our recent executive meeting it was decided to increase the membership fees. Paid Chaplains – £30, Chaplaincy Volunteers – £15.
This can also be done by Bank Transfer – please contact our treasurer for the bank details – treasurer@nihca.co.uk. Please include your Name as the Payment Reference in order to identify your payment and email our treasurer to confirm you have paid by bank transfer.
Free training is available only to chaplains who have paid their membership fee.
We welcome new members so please ask your colleagues in chaplaincy to consider joining the NIHCA.
All new membership applications require support by a Line Manager and then acceptance by the Executive Committee.
A membership application form must be approved before payment is made. You can find that here: https://www.nihca.co.uk/join-us/
European Network of Healthcare Chaplains
18th Consultation of the European Network of Healthcare Chaplains Consultation in Prague.
The U.K. group of chaplains are keen to share what they have learnt at the Consultation. It would be good if as many chaplains as possible could join us for this sharing session.
Find out more by joining the Teams session on Thursday 23rd May 1030-1130am. Login details are in email sent from Michael McMillan on May 1st 2024.
Job Opportunity
The Western Health and Social Care Trust are advertising for a Lead Chaplain.
See the link for further details and how to apply:
https://jobs.hscni.net/Job/34648/whsctlead-chaplain-band-7#
UK Board of Healthcare Chaplaincy (UKBHC)
Lay Director position (voluntary role)
Letter as follows:
“The UKBHC has at least one exciting volunteer opportunity for anyone who can demonstrate commitment to supporting the highest standards of safe and effective Chaplaincy/spiritual care in UK health and social care.
Healthcare Chaplains promote pastoral, spiritual and religious wellbeing through skilled compassionate person-centred care. This is available to our patients, their families and carers, and to staff, volunteers and students. They enable people to celebrate according to their religion or belief within NHS and other healthcare settings, and support those facing very difficult situations such as the death of a loved one, psychosis, being diagnosed with life-threatening conditions and people who are receiving end of life care, as well as being alongside those who just appreciate having a listening ear or a time to chat.
The purpose of the UK Board is to safeguard the wellbeing of the public by ensuring that healthcare chaplains deliver the highest standards of safe and effective care. The Board do this by supporting and promoting the work of healthcare chaplaincy through:
a) maintaining a register of accredited healthcare chaplains, which is recognised by the Professional Standards Authority (PSA);
b) setting standards for education and practice;
c) giving guidance to the registrants on matters relating to their role; and
d) the provision of Professional Advisers in the filling of vacancies
The Board is currently seeking to add at least one volunteer Lay Director to our existing team.
Note that while registrants are not eligible to apply, we want to raise awareness of this opportunity and ask you to distribute this more widely to individuals, registrants and groups as appropriate.
Please see the attached Expression of Interest for further information and the website – UK Board of Healthcare Chaplaincy – UKBHC
We would particularly welcome interest from applicants who have experience and skills in governance and/or communication.
Kind regards
Derek Johnston (UKBHC Secretary)
c/o Department of Pastoral & Spiritual Care
Hull Royal Infirmary
Anlaby Road
Kingston upon Hull, East Riding of Yorkshire HU3 2JZ
United Kingdom
Lay_Director_Expression_of_Interest_2024
New Website – Bereaved NI
Please check out this animation, designed by DoH Press Office, to support the launch of Bereaved NI.
You can visit the site here: https://bereaved.hscni.net/
CHCC (College of Healthcare Chaplains) ‘Towards Greater Diversity in the Healthcare Chaplaincy Workforce’ Extended Consultation
Please find attached a document open for consultation – feedback can be given to our training director until Wednesday 27th March – via email at trainingdirector@nihca.co.uk.
It should be noted, amendments relating to the Northern Irish aspects have already been made.
Greater_Diversity_CHCC_workforce_paper_consultation_format
St Patrick’s Pontifical University, Maynooth and Bon Secours Health System launch an Ethics module for ongoing professional staff training
Launch of Catholic Healthcare Ethics in the 21st Century.
Thursday 25th January 2024
St Patrick’s Pontifical University, Maynooth (SPPU), in partnership with Bon Secours Health System (BSHS), today launched a new Ethics module for those in Allied Healthcare, professional and administration roles, and people working in Pastoral Care or Chaplaincy.
The partnership announced last November provides ongoing professional development programmes suited to this group and those engaged in pastoral care roles in parish, diocese, or wider community settings.
The first module in this level 9 suite of programmes is Catholic Healthcare Ethics in the 21st Century. This for-credit module can be taken as a standalone short course or combined with further modules and a research project to attain a Postgraduate Diploma. Students will be able to select modules in the Ethics, Pastoral Care and Values-Based Leadership.
Each module, delivered through the SPPU online learning platform and by industry-leading professionals, offers the freedom to engage at a time that suits the learner.
Commenting at the launch, on the agreement to develop and deliver these programmes, President of St Patrick’s Pontifical University, Maynooth, Rev Prof Michael Mullaney, said: ‘Following the signing of the agreement between both organisations in November last, I am delighted to join Bill Maher and his team today to launch the first module in Ethics. At SPPU we see our role as being at the forefront of Catholic education and ensuring professionals in the field have adequate skills to make a real difference in the lives of those they serve. Our partnership with Bon Secours Health System is a further step on our collaborative journey with organisations who share our values.’
Bill Maher, Group Chief Executive Officer at Bon Secours Health System, added: ‘We are delighted to partner with SPPU, providing a bursary to develop a continuous education initiative in line with our mission to provide compassionate and exceptional medical care to those in need. This partnership is a step forward in advancing the education and training of healthcare and pastoral care professionals, offering them the opportunity to develop their ethical leadership, ultimately benefiting our national community.’
The development of these online programmes demonstrates SPPU’s commitment to delivering the highest levels of teaching and learning in order to promote intellectual, human and professional development. The programmes for Bon Secours Health System will be offered through the University’s Centre for Mission and Ministries.
(Source: https://sppu.ie/news-events/2024/sppu-maynooth-and-bon-secours-health-system-launch-an-ethics-module-for-ongoing-professional-staff-training)
You can read more about the course and how to apply on our Training Page: Training
Update Re AGM – Change of Date
Tuesday 28th May, T3 Conference Centre, House of Vic Ryn, Moira Road, Lisburn.
The AGM will take place on Tuesday 28th May between 9am and 2pm. We will start the business of the AGM at 9.30am sharp. Tea/coffee scones to start and finishing with lunch.
Clumsy to Bang Out of Order: Reviewing the UKBHC Code of Conduct

Paul Nash, one of the UKBHC Board Members, is currently leading a review of the UKBHC Code of Conduct. This is significant as the new NHS England Guidelines expect that all chaplains, registered or not, should abide by the code. Paul is keen to hear from chaplains, and from friends in other disciplines, reflecting upon your experiences, concerns, and those things that you think need updating or adding. Paul would also like to gather case studies that might go in the code or supporting documents. The QR code (above) links to a questionnaire (or the link below) you can fill in. If you would be interested in joining a small online working group for 3 hours over the next 6 months please contact Paul.
The 18th ENHCC Consultation
European Network of Healthcare Chaplaincy Conference
10th-14th April 2024
NIHCA members have previously attended this conference and found it to be very beneficial. See the invitation letter below. The NIHCA invites and will consider two grant applications covering travel and accommodation. Please respond to this email with your expression of interest and grant application detailing rough costings.
Belfast Trust Spiritual Care Week 16-20 October 2023
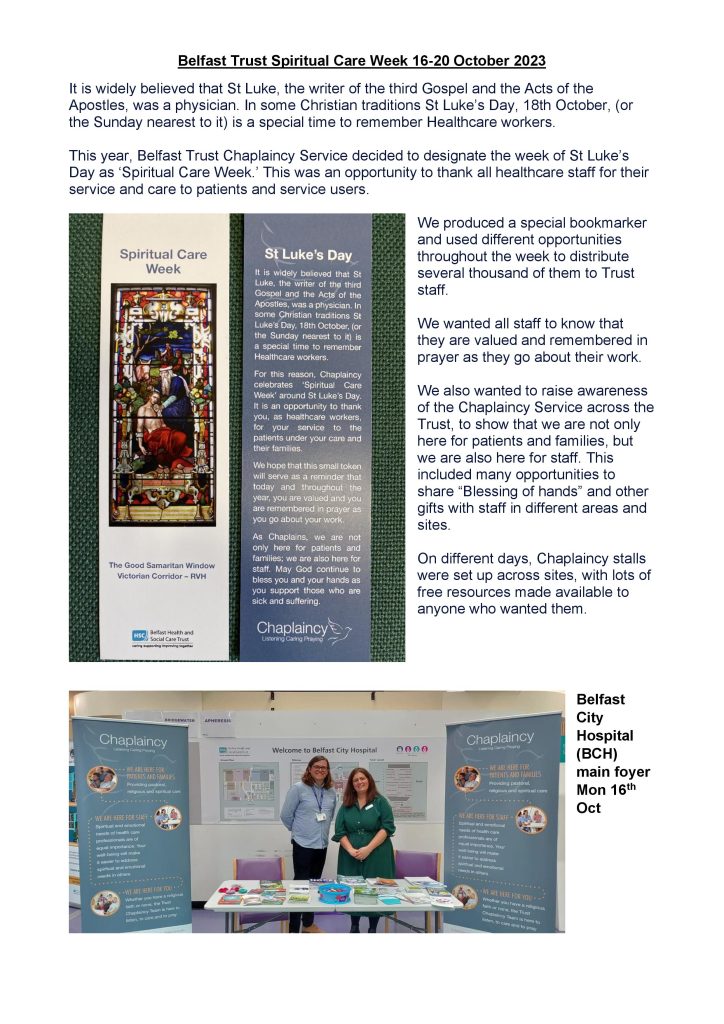

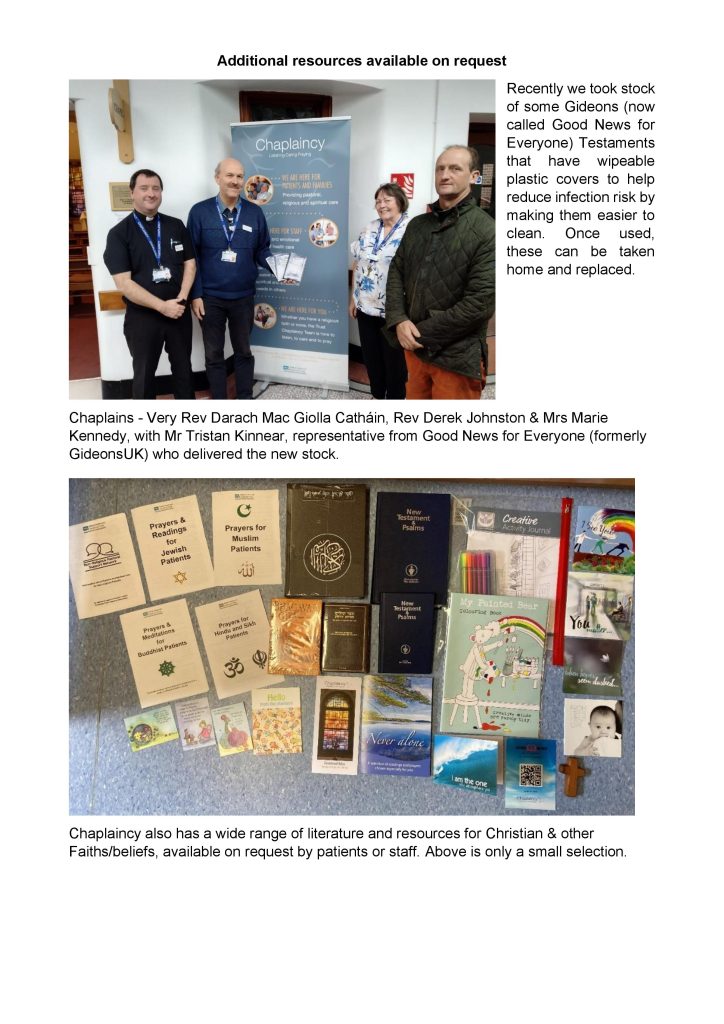
From the South Eastern Health & Social Care Trust
Our Chaplaincy team plays an important role, supporting patients and staff.
The Chaplaincy was delighted to welcome Presbyterian Moderator, Rev Dr Sam Mawhinney who was impressed with how staff work together in our Trust, putting patients at the heart of everything they do


“Multi-faith chaplaincy team is making a difference in acute hospitals”
Shropshire Council (UK) recently posted a news article about chaplaincy in the Shrewsbury and Telford Hospital NHS Trust. You can read the article here:
News from our partners: Multi-faith chaplaincy team is making a difference in acute hospitals
World Day for the Sick – Healthcare Chaplains Speak on Chaplaincy
This video has been produced by the Council for Healthcare of @CatholicBishops and you can contact informationHCBoard@gmail.com for more on a career as a Catholic healthcare chaplain.
Chaplains offer more than prayers:
New study confirms impact on ICU families
Read more about this new study here:
Chaplains offer more than prayers: New study confirms impact on ICU families
NIHCA – Past, Present & Future
The NIHCA Executive has approved a report on the NIHCA – its past, present and future. It will be forwarded to Chaplaincy line-managers, Department of Health and Church leaders.
You can download the report here (PDF):

First priority of Healthcare Chaplains is to ‘bring God’s compassion to those in need’ – Bishop Michael Router
Introduction
On 12 March 2022 at 12pm, Bishop Michael Router, Chair of the Irish Episcopal Conference Council for Healthcare, celebrated Mass in Saint Patrick’s College, Maynooth, for newly certified Healthcare Chaplains. The certification for Catholic chaplains is awarded by the Healthcare Chaplaincy Board, a sub committee of the Council for Healthcare.
Homily
The statement of Jesus in today’s gospel that we should “be perfect, therefore, as your heavenly Father is perfect”, is one of the most perplexing and challenging in the whole of the gospel. How can we be perfect? To be human is to be flawed in some way. It does not seem possible that we can achieve such perfection in this life. Yet this appears to be what Jesus is asking from us?
I believe that in making that very challenging statement Jesus is helping us see that faith in God is not just an occasional pastime or an intellectual exercise, but something that demands a transformation of our whole lives. We are called through our immersion into faith to mirror the very essence of God, not just in what we say and do, but in our way of being. If we can accomplish that then, despite our human weakness, we will reflect something of the nature of God to those whom we encounter.
Encountering others as people of faith is what each of you will do as healthcare chaplains, and indeed what each of us strive to do each day as Christians. If your presence is open and welcoming, if you have the ability to listen and to understand the physical, emotional, psychological and spiritual pain of others then you will have a transformational effect that will bring healing and hope into the most difficult and challenging situations.
The theme that Pope Francis chose for this year’s World Day of the Sick was “Be merciful, even as your Father is merciful”. Pope Francis tells us that “Mercy is God’s name par excellence”. In the Gospels we see Jesus displaying great concern and mercy for the sick. He made proclaiming the Gospel and healing the sick central to the mission of his disciples. People who are sick or in pain are isolated from others physically and in so many other ways.
This isolating nature of illness was heightened during the worst moments of the Covid-19 crisis. It served to highlight an element that is always present in the experience of ill health. Pain and suffering can bring loneliness, confusion and loss into the sick person’s life, and sometimes they can be as difficult to bear as the illness itself. That is why Jesus made healing and pastoral outreach to the sick an act of mercy and a crucial part of the Christian life. He touched the leper not just to bring healing but to highlight the importance of simple human connection in times of suffering. His gesture to those who were marginalised because of their illness brought them at once an experience of God’s presence and an understanding that they were not alone. It gave them the courage to face their situation and to hope for something new and life giving
That is why the journey you embark on as a Healthcare Chaplain has a vocational element. You are called to this work through your own lived experiences and through your own personal experiences of care and concern from others. Through a period of spiritual, theological, pastoral and personal formation you have each deepened your relationship with God and are ready to accompany others in their journey towards God. This is never done through preaching or through compulsion, but through a presence which helps others, in the circumstances of their lives, to encounter God.
You will face many challenges as healthcare chaplains. The role is increasingly coming under pressure from those who wish to exclude spiritual care and accompaniment from patient care and treatment. You will have to be sensitive to that reality, and negotiate your way around it, by once again modelling Christ in all that you do and say.
One positive aspect that the Covid-19 crises highlighted is the incredible work that is being done, each and every day, in our hospitals by so many dedicated professionals. To the forefront among that number are chaplains. The RTE Investigates programme ‘Covid-19: The Third Wave’, broadcast on the 9th February 2021, focused on the work of Tallaght Hospital during the height of the pandemic. The documentary highlighted in a special way the work of Fr. John Kelly, the head Chaplain, and his chaplaincy team. It brought to our attention the crucial nature of such work, not just in a crisis, but in the ordinary everyday life of such a busy healthcare facility. The spiritual and emotional care and support which the patients received from the chaplain was seen to be crucial in their treatment and holistic care.
The programme itself reflected a positive shift, during the pandemic in many people’s understanding of the chaplain’s work in the healthcare setting. As each of you begin your journey as a chaplain I know that you will continue to create that positivity about your role through your dedication and commitment to bringing the healing presence and power of Christ into every situation you encounter.
May God bless you in your work and may you see Jesus’ challenge to be perfect as your heavenly Father is perfect not as something impossible but as something that can be achieved when you allow yourself to be a channel of his grace, love, mercy, and healing to the weak, the suffering, and the poor who will be entrusted to your care in the years ahead.
Remember, your first priority will always be to bring God’s compassion to those in need. If you do the satisfaction and joy you will receive will bring you great fulfilment in your ministry and profession as a healthcare chaplain and as a representative of the Church’s ministry of healing.
Podcast – Reflections on Healthcare Chaplaincy in the UK
Personal reflections on Healthcare Chaplaincy in the UK by Canon Dr. Simon Harrison. Simon has worked delivering spiritual care in Acute and Mental Health Chaplaincy for over 20 years, and is heavily involved in the national Chaplaincy scene.
Latest episode is available here: https://anchor.fm/hospital-chaplaincy/episodes/6–what-makes-us-unique-in-what-we-do–and-how-do-we-get-better-at-it-e1iq2q2
Our New President & Training Director

We congratulate Rev Derek Johnston on his election as the President of the NIHCA and Mr Michael McMillan on his election as the Training Director of the NIHCA.
Inside, Outside, Upside Down: A hospital chaplain reflects on two years of COVID
Inside, Outside, Upside Down is the title of a children’s book written by Stan and Jan Berenstein to teach young children about spatial awareness. Over the years, this little, profound book has been adopted by adults to denote the topsy-turvy reality of life. When I was asked to reflect on the nearly two years of the COVID-19 pandemic, the title of this simple book immediately came to mind. As a hospital chaplain working in an academic health care center, providing care for the sickest people, I have often felt like the world has been turned “inside, outside, upside down.”
When the pandemic began, my first task as the director of spiritual care for the three hospitals in downtown Indianapolis was to decide how our department would respond to the anticipated patient needs. As non-clinical departments and personnel were encouraged to stay home and eventually work from home, we were faced with the same decision. As we reflected upon our role as chaplains, our department committed to stay on the units with our patients, their loved ones, and the staff. We believe our presence is important for the well-being, support, and care of everyone as we work to assure that compassion remain a hallmark of our care. Like military chaplains who go into combat with their units, our department made the gutsy decision to stay with our units, in our buildings, and with our people as the virus invaded our community.
Were we scared? Yes. Were we anxious? Very much so. Yet, this is our calling, and God never promised us it would be safe. For some of us, putting our health and lives on the line was a new consideration. We had bought into the community illusion that pandemics were a thing of the past. For others, especially those who had worked through the advent of HIV/AIDS epidemic, Legionnaires’ disease, H1N1 flu and had kept abreast of the warnings from epidemiologists, the pandemic – while concerning – appeared a bit more manageable because of these past experiences. All of us knew the risk of getting infected. There were no vaccines at that time, and we shared in our fear and anxiety.
As the supply of Personal Protective Equipment (PPE) such as masks, gloves and gowns dwindled, we had to make another quick decision. Would we be able to visit patients? The hospitals burned through our supply of PPE in less than a week. We quickly offered the chaplains refresher, hands-on education on the proper way to don (put on) and doff (take off) PPE. We had to improve our skill in following this procedure for our own protection and the protection of others. We limited our use of PPE, realizing that the patients needed the physicians, nurses and respiratory therapists at the bedside. This cut us off from our patients, pushing us to reset how we made visits.
As the shutdown of our communities went into effect, visitation by loved ones was prohibited. We immediately honed our technology skills utilizing virtual platforms in order help loved ones remain in contact with patients and their care teams. As chaplains accustomed to face-to-face visits, we were pushed into learning how to use our iPads and smart phones to maintain some connection between patients and their families. Quickly we realized we would be facilitating end-of-life conversations between physicians and families via a miniature video screen; not ideal. This was new, uncomfortable and anxiety producing for all of us. Yet, it had to be done to provide the compassionate care to which we are committed.
We stood with physicians, frustrated that the usual ways to treat lung infections proved futile in the presence of this deadly virus. The mucus in the lungs bound itself to the lung walls with such strength that respiratory therapists and pulmonologists (lung physicians) risked rupturing the lung wall with the suction used to remove it. The normal antibiotics seemed useless. Often in a matter of minutes patients would crash. Their lungs filling and their hearts pounding, they would suddenly die from the onslaught of the virus upon their bodies. Others would linger, their bodies fighting to ward off the virus as the respirators pushed air into their clogged lungs. Some survived; many did not.
The virtual visits continued from the doorways and hallways. After two weeks of being in the hospital, an older gentleman facing the decision to let his dear wife die from the disease asked to be able to see her one more time. As the chaplain held the iPad, he read Psalm 23 and, together, they said the Lord’s Prayer. The husband then said over the audio, “Love you, honey. See you in the stars. Goodbye.” He hung up the phone. The chaplain stayed with the staff who removed the respirator. A nurse said, “this is no way to die.” We were all heartbroken and scared. Our spirits were turned “inside, outside, upside down.”
In the early days of the pandemic the community rallied around us. We were self-conscious as cars filled with food and gifts came to the hospital declaring us “heroes.” The support was helpful, lifting our spirits as we faced days of death and destruction. A laundry in the city provided free laundry service for several weeks. It was a helpful perk since we had no time to wash our clothes. Church members from diverse congregations and faiths gathered on the lawns of our hospitals to pray for us and our patients. We felt encouraged, appreciated and empowered to keep showing up during that time. We were proud of our work, the care we provided, maintaining the compassionate presence. It was an upside of these early days. Today, that feels like it was in another era.
One of the big shifts for us has been the realization that the focus of our care was shifting to include the staff. We provided them with tranquility carts loaded with snacks, the most popular being chocolate. As the nurses said, “a tranquility cart without chocolate is just a cart.” There was no tranquility without chocolate. We provided Compassion Circles, organized by our continuing education team in partnership with the employee assistance program team; we utilized the Psychological First Aid and Critical Incident Stress Management intervention models to provide further support and care for employees. All the while, we kept hearing news of a vaccine. We hoped. We prayed. We kept doing our jobs.
As we came to the end of 2020, hope began to emerge. The vaccines were ready. We had a worship service to commemorate those who had died, support those who grieved and provide encouraging hope for all of us. In December, we began to receive the vaccines with applause, celebration and much fanfare. We were excited, renewed and full of hope as we entered a new year.
These were the “inside” days when we took a deep dive into the reality of a deadly pandemic that touched us all.
2021 became the “outside” year. The outside forces began to mount their resistance to the vaccine. Being the husband of a microbiologist and a student of epidemiology since contracting the H1N1 flu in 2009, I was surprised, shocked and stunned. As the son of an oral surgeon, I had been around medicine all my life. Medicine had saved my life from cancer at the age of 3. Medicine had provided for my well-being and education. My sister had become a medical librarian, and, prior to entering ministry, I was a sports medicine/physical therapy student. I knew, in layperson’s terms, the science behind the vaccine. Yet, the resistance grew. I was personally attacked when I posted on social media messages encouraging people to get the vaccine. I was told I did not trust Jesus and that my faith was weak.
Other members of my staff and their families suffered similar attacks. It was a bleak time for us all. As this happened the surges of the virus kept coming. People kept dying, and we continued to care for staff, patients and their loved ones. We fought back by finding a “new normal” through wearing masks, taking the vaccines and boosters, and continuing to limit our contact with others. All of us were touched by the spiritual and moral distress from this intense situation.
At the same time, we as chaplains stood in the paradox, in the land of Middle Earth, as Tolkien might say. We knew the science was valid: Messenger RNA science has been around for decades and is the basis for many of the cancer treatments we utilize today. We knew it was not a government plot or an evil manifestation. Yet, members of our churches, families and friends believed otherwise. We lived in the vice between these voices. These were the days of the “outside.”
The “outside” voices, fears, anxieties and ideologies seemed to be driving us into resisting the very things that could win this ongoing battle with the viral world. This was no time to blame. It was a time to thank God for the intelligence and understanding given to us to create a vaccine that could save us. Yet, we had to take the shot.
As a child of the 1950s, I found myself reflecting upon my childhood. I grew up with a friend who wore braces on his legs. Bobby used his crutches to walk to school faster than I could. As a person plowing through the ravages of polio, he found ways to survive and thrive. When the polio vaccine came about, we all lined up to take the droplet on a sugar cube. Our parents had lived through images of children in iron lungs and a president who could barely stand. There was absolutely no way any of us would not get the vaccine, no matter how novel it might be. What had happened to us, I wondered? Why are we so resistant? My only answer lay in the reminder of the powerful individualism and diminishing sense of community that continues to hamper our society and world. During these “outside” times, I grieved for the sense of community I enjoyed as a child: the strong Methodist and Presbyterian churches in which I was raised. My hope diminished during the “outside” days.
Throughout this time, chaplains continued to do their jobs. We enjoyed a few weeks and months when the virus slowed down. Then came the delta variant and, then, the omicron variant. Just today we learned they have merged into what is being called “delticron,” and we have patients with both COVID and the flu. The “inside” work goes forward. The “outside” battles continue. Yet, our world – our lives – feel turned “upside down.” Today, it feels like we live in an upside-down world.
This past week, one of our resident chaplains wrote a Twitter thread about his experiences. Rabbi Michael Harvey goes on in his thread to describe an event that took place during one of his overnight shifts. A patient had just died because of the virus. As he walked by the on-call nurse Michael asked, “Was he vaccinated?” The nurse responded, “I don’t know. I don’t ask any more.” As Michael says, “she’s right.” It does not matter. What is essential is that we provide all our patients and their loved ones with compassionate care. That is what we are all about. That is why chaplains are in our hospitals. That is our mission and purpose.
We are tired; physically and spiritually exhausted. While we are spent, the staff remains professional. The units remain calm in the face of an overwhelming number of patients, codes and deaths. When we cry, we weep. When we celebrate, it is with a smile or grin. We find ways to laugh with one another.
Physicians, nurses, respiratory therapists, environmental services, social workers and, yes, chaplains: We are all in this together. We care for our patients, their loved ones and one another — together. This faithful togetherness is the source of our resilience and strength.
Throughout this pandemic, we continue to be on our units and at the bedside. Chaplains have come alongside patients, their loved ones and the staff providing a comforting, supportive presence through overwhelming challenges. This is our mission, our purpose — our calling.
Today, my spiritual offering to our nursing staff was small beach balls in the break rooms and magnetic dart boards with an image of a coronavirus in the bullseye. Most of us no longer want or need to talk about the pandemic. We need to play and discover some kinetic release from the stress and strain of living in an “inside, outside, upside down” space. As Deuteronomy 30:19 reminds us, “I have set before you life and death, blessings and curses. Choose life that you and your descendants may live.”
There is life and hope as we journey through being turned “inside, outside, upside down.”
(Source: https://pres-outlook.org/2022/04/inside-outside-upside-down-a-hospital-chaplain-reflects-on-two-years-of-covid/)
“Healthcare is not just an organization; it depends on men and women who dedicate their life to taking care of other people’s health” (Pope Francis)
Hospital chaplains are central to “true healthcare”
Healthcare chaplains who provide spiritual nourishment to hospital patients are greatly appreciated and valued, the Moderator of the General Assembly has said.
Lord Wallace made the remarks during a visit to University Hospital Crosshouse, known locally as Crosshouse Hospital, near Kilmarnock to hear about their vitally important work.
He spent time with Andy Gillies, NHS Ayrshire and Arran lead for staff care, person-centred care and spiritual care, who gave him an overview of the service provided across the region.
“The role of the hospital chaplain is central to true healthcare,” said Mr Gillies. “They attend to needs that are beyond the medical, needs that makes a person a person.
“It was really good to have the Moderator and his wife visit the hospital and it symbolises that healthcare chaplaincy is taken seriously and is important.
“I am extremely grateful for Lord Wallace’s visit.”
Church of Scotland chaplains support patients, their families and staff in hospitals across the country.
Accompanying Lord and Lady Wallace on the visit was Barbara Urquhart DCS, a deacon and former hospital chaplain, and her guide dog, Inga.
Also present was Rev Jill Clancy, Moderator of the Presbytery of Kilmarnock and Irvine.
Lord Wallace is currently on a Presbytery of Irvine and Kilmarnock tour to learn more about the life and work of the local church.
Source: https://www.churchofscotland.org.uk/news-and-events/news/2022/articles/hospital-chaplains-are-central-to-true-healthcare
“I’LL MISS THE MIRACLES”
Today will mark the end of an era in the Diocese of Derry and Raphoe as Rev Canon David Ferry retires after 20 years’ service as a hospital chaplain in Londonderry. “I’ll miss the miracles,” the Tyrone man says of his “special calling”. He will be succeeded from tomorrow by the Rector of St Augustine’s Church, Rev Nigel Cairns.
Canon Ferry retired as Rector of the Balteagh group of churches in 2019 but carried on ministering to patients, families and staff in Altnagelvin and Waterside hospitals. It was a role he had first embraced under the late Bishop James Mehaffey.
“Chaplaincy’s a special calling,” Canon Ferry says. “It’s one of the ministries that Christ set apart – care for the sick, care for the disadvantaged – so to be called to that, and to be involved in that, always spoke to me about some sort of special vocation. It’s just an enormous privilege. To be with people, to hear people’s stories, to have the end of life conversations with people, to be the last person to say a prayer with them, it’s an amazing privilege.”
The last two years have been particularly trying, given how Covid has affected hospitals. Canon Ferry and his colleagues found themselves supporting not only patients and relatives, but staff too. “That was a big part of it, but I think their lives were being refined too. There’s nothing like a good furnace to do a bit of refining – so Scripture tells us. There was a whole mixture of bad things [during Covid] but, in that, there was a whole lot of good stuff happening as well, an awful lot of good stuff.
“The last two years tested your vocation,” Canon Ferry concedes. “Everybody in the hospital was tested, whether they knew it or whether they didn’t. Nurses in here were trying to organise not only their nursing life but home education for their children, so everybody was tested.
“We [chaplains] did the same thing [we always did] but we just did it differently. We had FaceTime with patients. That to me was so far removed from how I would do ministry – I take people by the hand, but we couldn’t do that. The staff were very good, though; they kept us all safe; they advised us what PPE to use. Families really appreciated it. We would make a telephone call. I found it very difficult because it wasn’t the way I operated, put it that way. But you’d say to the family, put your phone on speaker and I’ll pray for you all. And it didn’t matter where they were sitting – they could be at home – and I’d say put your phone on speaker and I’ll pray for you all. It was different. It was very different.”
Hospital chaplains are confronted with death and serious illness on a daily basis, but Canon Ferry says the relentlessness never got him down. “As Christians, we’re called to a great hope,” he says. “The world tells us that death is the end of all things. As a Christian, as a Christian chaplain, my hope is – for them, and for me – that death is not the end. Death is an experience we will all have in life. It’s the only thing in life that makes us all equal. But it’s not the end. Whenever you are there with a family and can reassure them through scripture – ‘In my Father’s house are many mansions and I’m going to prepare one for you’ – whenever you bring people to that sort of understanding, then death becomes….different.”
The prospect of retirement holds little appeal for Canon Ferry. “I’ve no clue about what retirement’s going to be like,” he says. “I’ve always tried to live each day in God’s plan as best I can, but it’s not something I’m really looking forward to. I’d love to have a gripe about the Bishop, or the Church or the hospital – it’d make it easier to go – but I don’t. I never ever had a gripe. I don’t know what a gripe is. I’m sure it’ll be great some morning when it’s teeming out of the heavens and I don’t have to get up.”
Will he miss chaplaincy work? “Oh aye. I’ll miss the miracles,” he says. “You see, as a hospital chaplain, every day you see the lame walk, the blind see, the deaf hear and the dead raised. You see those miracles every day. Somebody comes in here not able to walk, they go down to surgery, in two days they’re skipping. They come in here, they can’t see, [surgeons] take off their cataract and they see the very best. Put a hearing aid in…we have become so used to that, and we don’t see the miracle.
“I’m not going to start preaching but I think we need to look, we need to see the miracles. I often say – it’s a Presbyterian thing – but I always say you need to see the burning bush. There’s loads of them [miracles], loads of them, so I’ll miss the miracles. I’ll miss what the patients teach me: they teach me to be thankful, to appreciate the people I need to appreciate.
After twenty years in the hospitals, what in his opinion are the qualities that make for a good chaplain? “I think a good chaplain needs to stay out of God’s way and to know that we’re neither in control nor responsible,” Canon Ferry suggests. “I’m not in control of your life, I can’t keep you alive no matter what prayers I say. If it’s God’s decision that you’ll pass away today then you’ll pass away today. It’s my job to tell you that: God’s in control, not me. And I’m not responsible for you if you pass away; I’m not responsible for where you end up eternally. My responsibility – as the good book tells us – my job is to stand in the gap between God and his people, and as a chaplain that’s what I do, I stand in the gap between God and the patient.”
Canon Ferry has certainly earned his retirement. From tomorrow on, the task of ‘standing in the gap’ between God and the patients in Derry’s hospitals will fall to the Rector of St Augustine’s Church, Rev Nigel Cairns.
During his training for the ministry, the new chaplain watched his predecessor at close quarters, so he has a good understanding of what he’s letting himself in for. “I did a placement with Canon Ferry,” Nigel says. “It’s a frighteningly big commitment, but I enjoyed hospital chaplaincy very much. I appreciated the opportunity to journey with people through the worst of times and through the best of times.
“Miracles do still happen,” Nigel says, “and sometimes hospitals are the places where we see them occurring.
“I regard it as a great privilege to step into Canon Ferry’s shoes. I would like to acknowledge the loyal and dedicated way in which David has nurtured and developed the role of chaplain, widening it to include not only patients and families but the hospital staff too. The importance of that was very evident during the pandemic.”
Bishop Andrew has paid tribute to the outgoing chaplain and offered words of encouragement to his successor. “Canon David Ferry’s ministry to the sick and dying, to anguished relatives, and to hardworking staff in our hospitals has been of enormous comfort, often at the most difficult moments in people’s lives. In particular, I’d like to acknowledge the immense work he and his colleagues did during the pandemic, when hospital visiting was severely restricted. I thank God for the many qualities David has which equipped him perfectly for the role of chaplain. Our Diocese is immensely grateful for all that he has done to further God’s kingdom.
“Obviously, David is a hard person to replace, but I am confident that in Rev Nigel Cairns we have found a worthy successor. Nigel has many of the same pastoral gifts as David, and I have no doubt that patients, families and healthcare staff will benefit greatly from his care and support as chaplain.”
On the Bookshelf –
‘In the Midst of Life: Insights from a Hospital Chaplain’
by Paul Evans
A Tenby born Reverend, who now works in the health sector, has published a book called ‘In the Midst of Life: Insights from a Hospital Chaplain’.
Rev’d Michael Marsden (pictured) who was born and brought up in Tenby and attended Greenhill School, was ordained in Llandaff Cathedral in 1982 and has worked in a number of church and health care settings throughout South Wales.
He presently works within the Aneurin Bevan University Health Board, and is involved in nurse training and lectures regularly at the University of South Wales.
Married to Salli with two adult daughters, Lydia and Lucy, and a Parson Jack Russell called Toby, Rev’d Marsden’s book covers over 30 years’ experience working in health care as a chaplain, ministering to a countless number of patients, their families and health care staff.
In addition to these moving stories, each short, self-contained chapter contains a passage of scripture and prayer to assist the reader to reflect and ponder.
The Foreword has been written by Archbishop Rowan Williams, (formerly Archbishop of Canterbury): “I can’t think of another book that so beautifully sums up the vocation of a hospital chaplain, with a wealth of personal recollection and a wealth of invaluable quotation and reflection…. Michael writes with wit and clarity and compassion not simply about sickness and health but about the amazing grace of being human, and the joy of witnessing to this,” wrote Dr Rowan Williams.
Rev’d Lance Sharpe, Registrar, College of Health Care Chaplains, also said:
“When reviewing this book, I imagined it to be just another book on healthcare chaplaincy. However, I was pleasantry surprised as I was instantly struck by the personable tone that Michael writes in and the wisdom contained in the text is clearly borne of many years’ experience of frontline chaplaincy.
“The reflections and stories Michael uses in the book resonated deeply with my own experiences as a chaplain and certainly reminded me of the highs and lows that travelling alongside patients and reiterates the absolute privilege it is to share in their journey.
“I also appreciated the devotional and prayerful style that Michael employs in the book too. Using scripture, poems and prayers I can see this book being a useful resource for those involved in chaplaincy and pastoral ministry and as a valuable insight into the chaplain’s ministry for those exploring a vocation in this field…I am confident it will connect with all those involved in this work whatever their position or experience.
“I would wholeheartedly recommend this book for anyone interested in healthcare ministry.
‘In the Midst of Life: Insights from a Hospital Chaplain’ is now available to purchase on Amazon for £7.99.
(Source: https://www.pembroke-today.co.uk/article.cfm?id=130994&headline=On%20the%20Bookshelf%20-%20%E2%80%98In%20the%20Midst%20of%20Life:%20Insights%20from%20a%20Hospital%20Chaplain%E2%80%99§ionIs=news&searchyear=2021, accessed 11 May 2021)
From CNN, by Robert Klitzman
The ‘Amazing Grace’ of chaplains in the pandemic
“No one should ever have to die alone — to take their last breaths and say goodbye to the world by themselves with no one beside them,” a hospital chaplain recently told me. “With Covid, seeing patients dying alone has become the hardest part of my job. At the beginning of the pandemic, I saw even children dying alone.”
In the initial surge of cases last year, hospitals commonly banned all visitors. Family members of Covid-19 patients could themselves be infected and spread the virus to others when visiting their loved ones. Last summer, some hospitals, like Northwestern’s, started to let families visit to say goodbye if these loved ones agreed that doctors could write Do Not Resuscitate (DNR) orders, which mean forgoing so-called heroic measures. Yet this approach raises disturbing questions of whether families may feel coerced to agree to these terms in order to see their loved ones.
In trying times like these, chaplains, who provide spiritual care and support to patients, families, doctors and nurses, have bravely and tirelessly stepped up. Struggling on the front lines, helping to fill the gaping void that health care workers couldn’t, chaplains spoke to families, wrote these relatives’ messages to their loved ones on pieces of paper and handed these to nurses to read aloud in the patients’ rooms. Once chaplains were able to obtain appropriate personal protective equipment (PPE), they entered patients’ rooms with disinfected iPads and iPhones to let more people communicate with those in the hospital.
Chaplains still sit with innumerable dying patients to aid them and be there for families in decisive and painful moments. These spiritual care providers help patients and families alike to find meaning, purpose and hope when confronting death, and frequently mediate conflicts between patients and the medical staff.
Contemplating religious questions when confronting mortality is hardly new. In past epidemics, such as the Middle Ages’ devastating Black Death, massive numbers of people facing widespread disease, fear and death commonly turned to faith. But over the past few decades, America’s religious landscape has been dramatically shifting.
Across Christianity, Judaism and Islam, attendance at religious institutions has been steadily declining over the last two decades. Once, religions uniquely offered explanations for how species, the earth and the universe were created. But increasingly, science has provided reasons, with clear evidence. In addition, people now more readily question authorities, whether political or religious, and the Internet, social media and globalization, have exposed people to wide ranges of beliefs that differ from the traditional faiths with which they may have been raised. Moreover, whereas houses of worship once allowed people to interact and connect outside of work at set times, social media now serves similar functions any time or day.
Covid-19 has also transformed religious and spiritual practices. Many people cope with stress by spending time with family and friends, and going to gyms, churches, temples, restaurants, bars, theatres and stores. But the pandemic has stymied these activities and connections to others. Many of us have been forced to reconsider what is truly important in our lives, to question the meanings of our daily routines, work, relationships and goals. We have often relinquished activities and interactions that now, on reflection, don’t feel as meaningful. Religious services have also moved online and been reduced to two-dimensional electronic screens, lacking vital human touch.
Hospitalized patients and their families face these challenges even more acutely, and healthcare providers have had to devise new, creative responses and interactions. Especially in the pandemic’s early days, doctors and nurses were stretched thin and frequently had little PPE. They tried as much as they could to address patients’ spiritual and existential needs, occasionally filling some of the roles of hospital chaplains, arranging Zoom calls with shocked, grief-stricken family members. But doctors and nurses could not do it all, and many have felt burnt out themselves, making chaplaincy services critical.
Health care, however, is a big business and many hospitals still underappreciate, understaff and underfund chaplaincy departments, which insurers do not reimburse , and which therefore do not directly generate revenue. In 2015, 70% of over 4,000 US hospitals surveyed by the American Hospital Association offered chaplaincy and pastoral care services, up from 53% in 2002. But more are needed.
Many doctors also remain wary of addressing spiritual, religious and existential issues in medical care. Even with patients who have advanced cancer, 47% of physicians feel personally uncomfortable discussing spiritual issues with patients, and 45% think it is not their professional role to do so. Sixty-two percent of doctors say they have not received adequate training in this area. Yet among US medical school deans, only 7% said that their schools offered required coursework dedicated to spirituality and health, and only 21% thought that it would be important to develop national standards for competencies in training on issues regarding spirituality and health. Even if they received funding and assistance, only 25% would make additional time available in the curriculum for these issues.
Research shows, however, that patients who see a chaplain during their hospitalization, whether they initially wanted to or not, rate their overall satisfaction with their hospitalization higher. And some research suggests the presence of such services is associated with fewer hospital deaths. Alas, many hospitals and physicians feel that these studies are not enough.
Much of what chaplains do, however, lies beyond financial metrics. Covid-19 has in fact shown how chaplains can play increasingly vital roles, and how patients’ needs for meaning and hope extend beyond profit alone.
Recently, for instance, a chaplain told me of a dying 12-year-old who wanted to be an organ donor. After he was declared brain dead, the doctors would need to wheel him into the operating room, and then disconnect his life support to quickly “harvest” his organs while these tissues were still viable. The family wanted to be present when he took his last breath. But the doctors feared that the family would become upset, and thus delay the ability to remove the organs in a timely way. The family and the doctors argued and couldn’t resolve the tension.
The chaplain spoke at length to the family, who agreed to be in the OR for only three minutes. Once in the room, all garbed in sterile gowns, she asked them whether their son had a favorite song. The mother said, Amazing Grace. The family then sang it, with the doctors and nurses joining in. Everyone cried, including the staff.
After that the family left. A few days later, the chaplain phoned the mother to see how she was doing. “Thank you for that gift,” she said. “We will never forget that. We got to sing my son into Heaven.”
Hopefully, none of us will ever forget the pandemic’s lessons regarding the importance of chaplains and of patients’ and families broader spiritual, religious and existential needs beyond the biomedical alone.
(Source: https://edition.cnn.com/2021/04/19/opinions/frontline-worker-pandemic-chaplain-klitzman/index.html; accessed April 27, 2021)
Additional funding to support hospital chaplains
Health Minister Robin Swann has announced an additional £25,000 funding to support the work of the Northern Ireland Healthcare Chaplains Association (NIHCA).
Chaplains are employed directly by HSC Trusts to provide spiritual care to all patients, visitors, staff and volunteers across healthcare, regardless of faith or no-faith.
Commenting on the funding the Health Minister said:
“I am delighted to be able to offer this additional funding to the Northern Ireland Healthcare Chaplains Association. I want to pay tribute to the work of our hospital chaplains. They have provided spiritual and religious care, support and comfort to patients, their families and healthcare staff, during some of the bleakest moments in this pandemic. Often chaplains have been the only non-clinical faces seen by patients, delivering much needed support with dignity and compassion.
“This extra funding will provide much needed additional professional training for chaplains and the development of a local bank of practical resources for use by patients.”
He also thanked the NICHA for its ongoing and active role in equipping chaplains to undertake their important role.
Rev. Norman Harrison, Director of Training for the Northern Ireland Healthcare Chaplains Association, stated that:
“The NIHCA very much welcomes and appreciates the acknowledgement which this funding represents of the work of Chaplains throughout the pandemic across all the HSC Trusts. We would like to thank the Minister as well as the Department of Health for giving both time and consideration to Chaplaincy, and for the encouragement this tangible acknowledgment brings, as we pursue our goal of preparing Chaplains for their professional role within the HSCNI.”
The Department of Health currently provides annual funding of £33,000 to the NIHCA to support the training and development of chaplains.